Table of Contents
Introduction
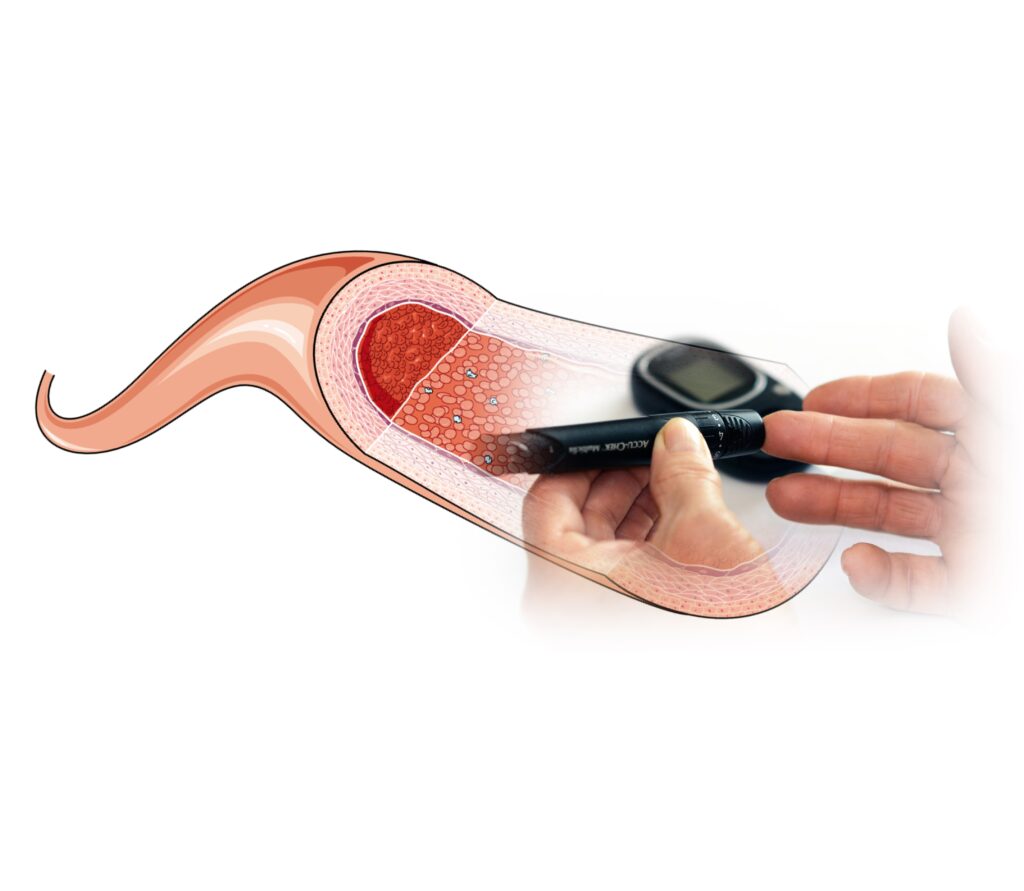
Diabetes is a chronic condition that affects millions worldwide, characterized by elevated blood sugar levels. Over time, uncontrolled diabetes can lead to various complications, including damage to blood vessels throughout the body. Understanding how it impacts blood vessels is crucial for managing the condition and preventing complications.
When blood sugar levels remain consistently high, it can result in the thickening of blood vessel walls and cause them to become less flexible. This can impede proper blood flow, leading to an increased risk of cardiovascular diseases such as hypertension, heart attack, and stroke. Additionally, the tiny blood vessels in the eyes, kidneys, and nerves are particularly vulnerable to damage from high blood sugar levels. In the eyes, this can lead to diabetic retinopathy, a leading cause of blindness. In the kidneys, it can cause diabetic nephropathy, potentially leading to kidney failure. Diabetic neuropathy, affecting the nerves, can result in pain, tingling, or loss of sensation, particularly in the extremities. Hence, it is vital for individuals with diabetes to maintain proper blood sugar control and undergo regular health check-ups to monitor and manage these risks effectively.
Mechanisms of Damages due to Diabetes
Advanced Glycation End Products (AGEs):
Advanced Glycation End Products (AGEs): High blood sugar levels in diabetes can lead to the formation of AGEs, which are harmful compounds that accumulate in tissues. AGEs contribute to blood vessel damage by promoting inflammation and oxidative stress. This accumulation not only affects the blood vessels but also interferes with normal cellular functions and can accelerate the aging process. AGEs can also cross-link with collagen in blood vessels, further reducing their elasticity and impairing their ability to function properly.
Oxidative Stress: Diabetes increases oxidative stress in the body, causing an imbalance between free radicals and antioxidants. This oxidative stress damages the lining of blood vessels (endothelium), impairing their ability to regulate blood flow and causing inflammation. Over time, the chronic oxidative damage can lead to a breakdown of the endothelial barrier, increasing the permeability of blood vessels and contributing to the development of atherosclerosis and other vascular complications.
Increased Blood Pressure: Diabetes can lead to high blood pressure (hypertension), which puts strain on blood vessel walls. Persistent hypertension can cause structural changes in blood vessels, making them less elastic and more prone to damage. The increased pressure can also exacerbate the effects of other diabetic complications, such as retinopathy and nephropathy, by further stressing the delicate blood vessels in the eyes and kidneys, leading to a vicious cycle of damage.
Types of Vascular Damage
Atherosclerosis: It accelerates the development of atherosclerosis, a condition where fatty deposits (plaques) build up inside arteries. These plaques can narrow and harden arteries, reducing blood flow and increasing the risk of heart attack and stroke. The presence of AGEs and oxidative stress in diabetes further exacerbate plaque formation and instability, making atherosclerotic events more likely. Learn more about atherosclerosis here.
Microvascular Complications: It damages small blood vessels, affecting organs such as the eyes (leading to diabetic retinopathy), kidneys (diabetic nephropathy), and nerves (diabetic neuropathy). These complications result from reduced blood flow and impaired nutrient delivery to tissues. In the eyes, for instance, microaneurysms and hemorrhages can occur, while in the kidneys, damage to the glomeruli impairs filtration, leading to proteinuria and eventually chronic kidney disease.
Peripheral Artery Disease (PAD): It increases the risk of PAD, a condition where narrowed arteries reduce blood flow to the limbs. PAD can lead to pain, numbness, and in severe cases, tissue death (gangrene). Diabetic patients are particularly vulnerable to PAD due to the combined effects of atherosclerosis and microvascular damage, which compromise blood flow to the extremities, making them more susceptible to infections and slow healing. Explore more about PAD here.
Preventive Measures and Management
Managing diabetes effectively is key to preventing vascular damage. This includes:
·Blood Sugar Control: Monitoring blood sugar levels and adhering to a management plan prescribed by healthcare professionals. Frequent glucose monitoring helps in making timely adjustments to diet, exercise, and medications, ensuring optimal blood sugar control and reducing the risk of complications.
·Healthy Lifestyle: Adopting a balanced diet, regular physical activity, and avoiding smoking to reduce cardiovascular risk factors. A diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and can help manage weight, while regular exercise improves cardiovascular health and insulin sensitivity.
·Medication: Taking prescribed medications to control blood sugar, blood pressure, and cholesterol levels. Medications such as insulin, metformin, ACE inhibitors, and statins play a crucial role in managing diabetes and its associated risk factors, providing a comprehensive approach to preventing vascular damage. Regular follow-ups with healthcare providers ensure that treatment plans are adjusted as needed to maintain optimal health.
Conclusion
Understanding how diabetes damages blood vessels underscores the importance of proactive management and regular medical check-ups. By controlling blood sugar levels and adopting a healthy lifestyle, individuals with diabetes can mitigate the risk of vascular complications. Regular consultations with healthcare providers are essential for personalized management and early detection of any emerging issues.
Effective diabetes management requires a multifaceted approach that includes maintaining a balanced diet, engaging in regular physical activity, and adhering to prescribed medications. Monitoring blood glucose levels frequently allows for timely adjustments in treatment plans, ensuring optimal control over the condition. Additionally, lifestyle modifications such as quitting smoking and reducing alcohol consumption can further reduce the risk of complications. Education about diabetes and its potential impact on overall health empowers individuals to take an active role in their care. Support from healthcare teams, including dietitians, endocrinologists, and diabetes educators, can provide valuable guidance and resources. By staying informed and vigilant, individuals with diabetes can lead healthier lives and prevent the severe consequences associated with vascular damage.
References
·American Diabetes Association (https://diabetes.org/)
·National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (https://www.niddk.nih.gov/)
·Centers for Disease Control and Prevention (CDC) – Diabetes (https://www.cdc.gov/diabetes/index.html)

