Table of Contents

Introduction
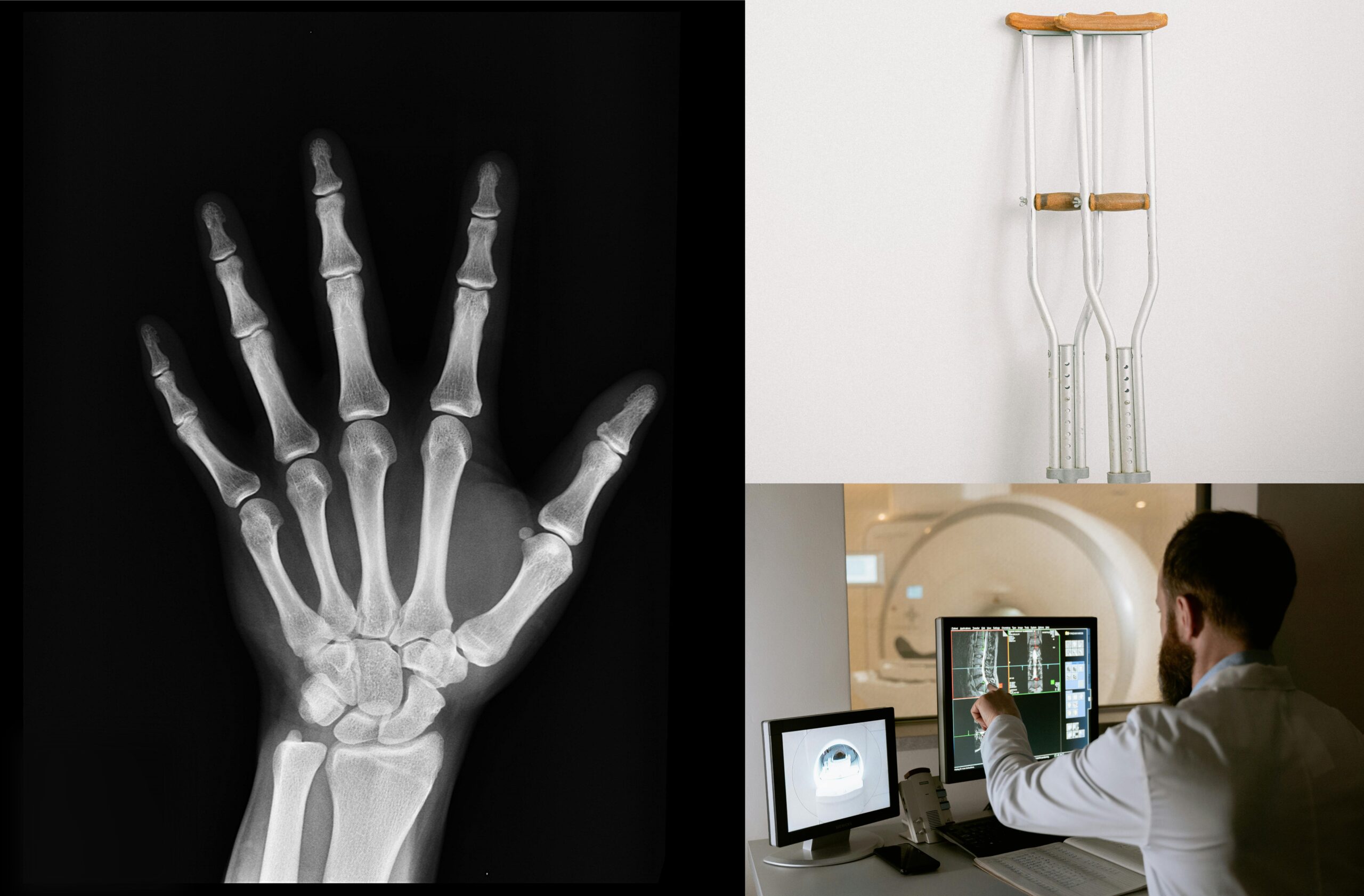
Bone fractures are among the most common injuries in humans. Whether from a fall, an accident, or high-impact sports, bones can break or crack. But the body has a remarkable ability to repair itself. From the moment a bone fractures or breaks, intricate biological pathways are activated to restore its structure and function. This article will walk you through how bone fractures heal over time, the stages of recovery, and what modern science reveals about the biological processes involved.
The Complexity of Bone Healing
The process of bone healing is complex and involves multiple stages. From the initial inflammatory response to the formation of new bone tissue, the body orchestrates a well-coordinated series of events aimed at restoring the bone’s integrity. Understanding how these processes work not only helps patients grasp the importance of post-fracture care but also provides insights into how modern medicine supports and sometimes enhances the body’s natural healing mechanisms.
Bones are not static structures. They are living tissues that continuously remodel and respond to the physical stresses placed on them. When a fracture occurs, the body must repair the broken tissue while maintaining overall balance in the skeletal system. This process requires the coordination of various cell types, signaling molecules, and biological pathways, making bone healing a complex yet fascinating phenomenon.
Stages of Bone Healing: From Break to Build
Inflammatory Stage (Days 1-7)
Immediately after a fracture, the body initiates the inflammatory stage. This stage serves two critical functions: protecting the injured area from infection and initiating the healing process.
- Hematoma Formation: When a bone fractures or breaks, blood vessels are also damaged, leading to the formation of a blood clot (hematoma) around the fracture site. The hematoma contains platelets, white blood cells, and other immune cells that release growth factors, signaling the need for repair.
- Inflammation: Inflammation follows, creating an environment conducive to healing. Immune cells clear debris, and signaling molecules recruit cells necessary for the next stage.
Reparative Stage (Weeks 1-6)
The reparative stage is when new tissue starts to form. The body begins the actual “building” process during this phase. Two sub-phases define this stage:
- Soft Callus Formation (Weeks 1-2): Specialized cells called fibroblasts and chondroblasts are recruited to the fracture site. They start producing a soft callus made of collagen and cartilage, temporarily bridging the broken bone ends. This tissue is weaker than bone but provides early stability.
- Hard Callus Formation (Weeks 3-6): Osteoblasts, cells responsible for new bone formation, replace the soft callus with a hard, mineralized callus made of woven bone. This stage strengthens the bone considerably, though it is still not as durable as normal bone tissue.
Remodeling Stage (Months 3-12)
The remodeling stage can last several months to years, depending on the size of the fracture and the individual’s health. During this phase, the bone becomes fully functional again.
- Bone Resorption: Osteoclasts, the cells that break down old or excess bone, remove the initial hard callus, creating space for more organized bone.
- Bone Remodeling: Osteoblasts continue to lay down new bone, refining its structure. The woven bone formed in the earlier stage is replaced by stronger, more resilient lamellar bone. The bone eventually regains its normal shape, and mechanical strength is restored.
Factors That Influence Bone Healing
The time it takes for a fracture to heal can vary significantly from person to person. Several factors influence the speed and success of bone healing, including:
- Age: Younger individuals typically heal faster than older adults, as cellular regeneration is more efficient.
- Overall Health: Conditions such as diabetes or osteoporosis can slow down the healing process.
- Lifestyle Choices: Smoking, poor nutrition, and lack of physical activity can negatively affect bone healing.
- Fracture Type: Compound fractures, where the bone breaks through the skin, are more prone to complications like infection, delaying healing.
- Medical Interventions: Sometimes, medical interventions like surgery or the use of bone grafts are required to facilitate healing, particularly in complex or non-healing fractures.
The Biology of Bone Healing: Molecular and Cellular Pathways
The Role of Growth Factors
Growth factors are proteins that play a pivotal role in bone healing by stimulating cellular activity. During the inflammatory and reparative phases, various growth factors are released to signal cell proliferation and differentiation.
- Bone Morphogenetic Proteins (BMPs): These proteins are crucial for the formation of bone and cartilage. BMPs recruit mesenchymal stem cells to the fracture site, where they differentiate into osteoblasts and chondroblasts, essential for new tissue formation.
- Transforming Growth Factor-Beta (TGF-β): TGF-β regulates the proliferation and differentiation of osteoblasts. It is instrumental in forming the soft callus, which is later replaced by hard bone.
- Vascular Endothelial Growth Factor (VEGF): VEGF promotes the growth of new blood vessels in the damaged area, ensuring that the healing tissue receives adequate oxygen and nutrients.
Stem Cells and Bone Healing
Stem cells, particularly mesenchymal stem cells (MSCs), are key players in bone fractures repair. These cells are multipotent, meaning they can differentiate into a variety of cell types, including osteoblasts and chondroblasts. During the reparative stage, MSCs migrate to the fracture site and contribute to the formation of both the soft and hard callus.
Modern scientific advancements have focused on enhancing the activity of MSCs to accelerate bone healing. Research into stem cell therapy and tissue engineering holds promise for treating complex fractures or conditions where natural healing is impaired.
The Importance of Mechanical Load and Bone Healing
One fascinating aspect of bone healing is its dependence on mechanical forces. The concept of “Wolff’s Law” states that bone grows and remodels in response to the stresses placed upon it. This principle is critical during the remodeling stage of healing.
Controlled weight-bearing exercises are often recommended after the initial stages of healing to promote bone strength. Mechanical load stimulates osteoblast activity, encouraging the replacement of woven bone with stronger lamellar bone.
Modern Interventions in Bone Healing
Bone Grafting
For fractures that do not heal naturally, bone grafting is a common intervention. Bone grafts can be harvested from the patient’s own body (autografts), a donor (allografts), or made synthetically. The graft serves as a scaffold for new bone growth and helps to bridge large gaps in fractured bone.
Stem Cell Therapy
Stem cell therapy is an emerging field in orthopedic medicine. By injecting MSCs into the fracture site, doctors can enhance the body’s ability to regenerate bone. While this treatment is still under investigation, early results are promising, especially for non-healing fractures.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves injecting a concentrated solution of the patient’s own platelets into the fracture site. Platelets are rich in growth factors that stimulate healing. This therapy has shown promise in accelerating the reparative phase of bone healing.
The Future of Bone Healing: Bioprinting and Tissue Engineering
The future of bone healing may lie in advanced technologies like 3D bioprinting and tissue engineering. Scientists are working on creating scaffolds that mimic the natural bone environment, encouraging cells to grow and form new bone tissue. These techniques could revolutionize how we treat severe fractures or bone diseases.
3D Bioprinting
3D bioprinting involves creating three-dimensional structures using a bio-ink made from cells and biomaterials. These structures can serve as a template for bone growth, potentially eliminating the need for bone grafts. While still in the experimental stage, 3D bioprinting holds tremendous potential for future applications in bone healing.
Gene Therapy
Another cutting-edge area of research is gene therapy. Scientists are exploring ways to manipulate the genes that regulate bone growth and repair. By activating or silencing specific genes, it may be possible to enhance the body’s natural healing processes, reducing recovery time and improving outcomes for patients with complex fractures.
Conclusion: The Resilience of the Human Body
Bone fractures may be common, but the body’s ability to heal and repair itself is nothing short of extraordinary. From the moment of injury to the final stages of remodeling, bone healing is a highly regulated and efficient process. Understanding the biological pathways behind this process not only offers insights into the human body’s resilience but also underscores the importance of proper medical care and rehabilitation. With modern scientific advancements like stem cell therapy and 3D bioprinting on the horizon, the future of bone healing is bright, offering new hope for patients with even the most challenging fractures.
Frequently Asked Questions (FAQs)
1. How long does it take for a bone fracture to heal?
It typically takes 6-8 weeks for a bone to heal, but this can vary depending on the individual and the severity of the fracture.
2. What are the stages of bone healing?
Bone healing occurs in three stages: inflammatory, reparative, and remodeling.
3. How can I speed up bone healing?
Adequate nutrition, rest, and following medical advice such as physical therapy can promote faster healing.
4. What role do stem cells play in bone healing?
Stem cells differentiate into bone-forming cells and are crucial for the formation of new tissue during the healing process.
5. Can fractures heal without medical intervention?
Some minor fractures can heal naturally, but most require medical intervention for proper alignment and to prevent complications.
6. What is the role of growth factors in bone healing?
Growth factors stimulate the proliferation of cells necessary for bone repair and regeneration.
7. Is surgery always required for bone fractures?
Not all fractures require surgery. Surgery is typically reserved for complex or non-healing fractures.
8. What is 3D bioprinting in the context of bone healing?
3D bioprinting involves creating scaffolds that promote bone growth and may one day replace traditional bone grafts.
References
https://www.ncbi.nlm.nih.gov/books/NBK551678
https://www.mdpi.com/1422-0067/20/22/5805
https://www.mdpi.com/2227-9059/9/7/748
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105171
https://www.mdpi.com/2306-5354/11/1/67 https://www.mdpi.com/1422-0067/22/2/767
YouTube video linkhttps://youtube.com/shorts/0eBwiA15JjY?feature=share

Your writing has a way of resonating with me on a deep level. It’s clear that you put a lot of thought and effort into each piece, and it certainly doesn’t go unnoticed.
Thank you so much for your heartfelt feedback! I’m thrilled to hear that my writing resonates with you. Your support means a lot, and I hope you continue to enjoy and share it with others.